Posts
Showing posts with the label Morgue
The Dead Don't Know The Difference Between Morgue or Trailer Outside,The Living Do
- Get link
- X
- Other Apps
One More Crisis in America: Overflowing Morgues! Do You Need To Care?
- Get link
- X
- Other Apps
Breaking News}} FEMA Denies PR Help To Help Process The Accumulation of Bodies
- Get link
- X
- Other Apps
PR Governor: We Need to Solve The Century Old Problem of Colonialism
- Get link
- X
- Other Apps
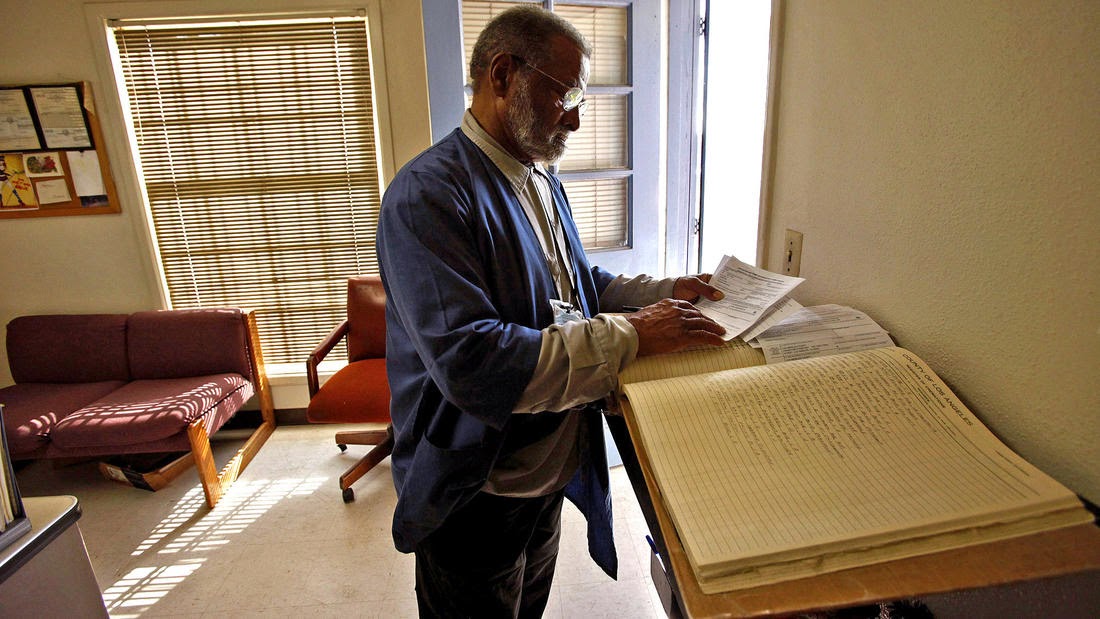
Unclaimed Dead Awaits a long Final Send Off at LA County Cemetery
- Get link
- X
- Other Apps