Posts
Showing posts with the label HIV/Undetectable
If You Tested HIV Positive But are Undetectable, Should You Tell A Sex Partner
- Get link
- X
- Other Apps
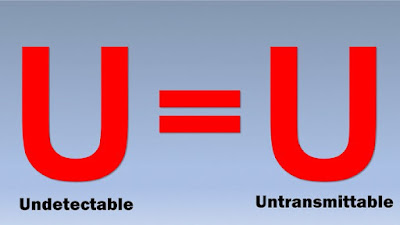
What is HIV undetectable = untransmittable (U=U)?A Viral Load Will Tell The Tale, I'll tell U More
- Get link
- X
- Other Apps
19 Yr Old Diagnosed with HIV in Feb This Yr., WHY? What is it We Don't Know?
- Get link
- X
- Other Apps
You R Going to Bed with a cutie on his word. Ur negative. if he is undetectable ASK.and See
- Get link
- X
- Other Apps
If You Are LGBTQ and Run Away from HIV You Are The Problem
- Get link
- X
- Other Apps
Details of The Second HIV-Free Patient With Stem Cell Treatment
- Get link
- X
- Other Apps