Posts
Showing posts with the label HIV Aids
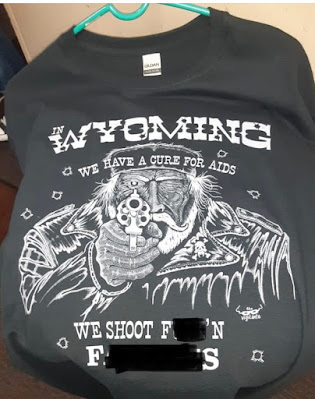
Gay Eagle’s Nest Sells T Displaying Gun As The Answer for People With AIDS✏
- Get link
- X
- Other Apps
Deaths From HIV/AIDS Have Continued to Drop According to CDC Study
- Get link
- X
- Other Apps
Improvements in 40 Yrs on HIV-AIDS But Stigma Remain and Because of It HIV Remains
- Get link
- X
- Other Apps
Tommy La Sorda' Son with Nonacceptance of His Sexuality, Early Death and AIDS
- Get link
- X
- Other Apps