Posts
Showing posts with the label HIV Cure
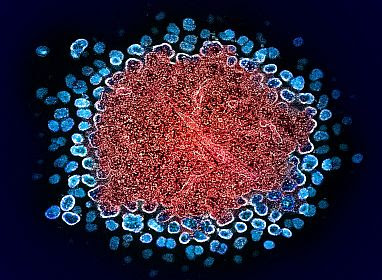
There is a ‘Cure’ For Not Turning HIV But Why 50% Blacks Don’t Have it
- Get link
- X
- Other Apps
He is 67 Diagnosed Not HIV but AIDS at 33 (1988) Today He is Totally Cured
- Get link
- X
- Other Apps
Another Case of HIV Total Cure on a Woman Receiving Stem Cells
- Get link
- X
- Other Apps
66 Yr Old Man Totally Cured of HIV After 3 Years of Transfusions
- Get link
- X
- Other Apps
Steps Toward HIV Total Cure (5 Cured Already)
- Get link
- X
- Other Apps