Happiness Comes From Within {Release of Serotonin}
‘Folks are usually about as happy as they make up their minds to be’ – Abraham Lincoln.
Happiness comes from within. More specifically, from the brain. Surely I am biased when I say the nervous system is incredibly interesting, but I am not the only one who thinks this. The public’s fascination with the brain most likely comes from the fact that it shapes things as intangible as behavior, mood, and decision‐making.
And here is where one of my favorite molecules comes into play: serotonin.
Serotonin (5‐HT) is a neurotransmitter that comes from breaking down tryptophan, an important amino acid that we need to acquire from our diet, as our body is unable to produce it. Serotonin is not exclusively found in the central nervous system (CNS) but also in the gastrointestinal tract (which is its main location) and blood platelets. Together with dopamine, serotonin is mainly known for making us happy. But serotonin is also in charge of other functions. Many studies have shown that mice lacking this important neurotransmitter exhibit some characteristic behavioral traits, for instance: mice were more aggressive than usual towards new (unknown) mice, pups were heavily neglected (and often attacked) by their moms, and male mice did not seem to care about the genderof their sexual partners. All of the studies that have been carried out are very exciting, and clearly, show the importance of serotonin in both our social interactions and behavioral states.
What makes you happy?
As mentioned above, serotonin has long been linked to happiness, and with its buddy, dopamine, these two neurotransmitters, among many other functions, are in charge of keeping us content.
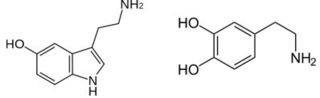
Serotonin and dopamine
Source: No copyright
Serotonin is released from the pre-synaptic neuron and binds to its receptors and its transporters (called SERTs) on the post- and pre-synaptic neuron. When serotonin binds to the receptor on the post-synaptic neuron, it triggers neurotransmission and it can cause, among other effects, the ‘happy’ feeling. In contrast, when serotonin binds to the SERT on the pre-synaptic neuron, it causes the internalization of serotonin back into the pre-synaptic compartment, where it is degraded or accumulated in vesicles. The interaction of serotonin with its transporters at the pre-synaptic neuron decreases the release of serotonin in order to control the concentration of serotonin at the synapse.
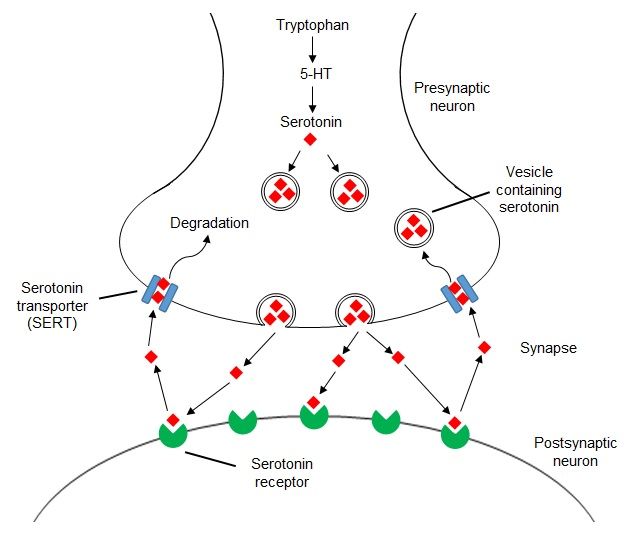
Serotonergic synapse
Source: Elena Blanco-Suarez
SERTs are popular targets of anti-depressant medication, like the SSRIs (selective serotonin reuptake inhibitors). For example, the world-famous Prozac (fluoxetine) belongs to this family of anti-depressants. The function of SSRIs is to block the clearing of serotonin from the brain. More specifically, the SSRI blocks the reabsorption/reuptake of serotonin at the pre-synaptic neuron in order to leave serotonin around for longer. The result is that more serotonin is available to the neurons, and we feel more cheerful.
Emotional serotonergic rollercoaster
There are studies in healthy individuals that show that serotonin activity actually varies during the day, and can even depend on the season. However, more severe cases can lead to seasonal affective disorder (SAD), full-blown depression, or a wide range of other mood disorders. We cannot say though that serotonin is the sole reason for depressive or euphoric states. There are many factors (as usual, when it comes to the brain) that determine and modulate this. There is strong evidence, however, that maintaining a higher level of serotonin in the brain helps with symptoms of depression.
Furthermore, a recent study has found that in moms suffering from post-partumdepression (PPD) there is a remarkably high level of monoamine oxidase A (MAO-A), the enzyme that breaks down serotonin, but also dopamine and its product norepinephrine. So the high levels of this enzyme (an astonishing 40% more in moms with PPD than in women who have not given birth lately) contribute to destroying the serotonin that would be helping the new mom feel as wonderful as society expects her to be. Researchers are working to develop possible treatments for the serious threat of PPD and also, an easy way of detecting such enzymatic overload in the brains of the new moms in order to quickly and accurately diagnose PPD. Treating PPD with SSRIs might not be the best way to go: it is true that they raise the levels of serotonin by blocking the reuptake, but they may ignore other effects that come from the high concentration of MAO-A, like degradation of other substrates such as dopamine and norepinephrine. Therefore, the use of selective and reversible inhibitors of MAO-A (MAOIs) could be more effective than using SSRIs for the treatment of PPD. SSRIs are, however, still the most common medication to treat depression and other mood disorders.
Drugs like 3,4-methylenedioxymethamphetamine (better known as MDMA or ecstasy) also mess with your serotonin levels by targeting SERTs. MDMA use will overflow your brain with serotonin (along with dopamine and the hormones oxytocin and prolactin), which is why you feel awesome when under the effects of this drug - MDMA is not called ecstasy for no reason. The problem comes later when the “nice” effects of the drug wear off and you feel the comedown. This is your brain lacking serotonin due to the high usage a few hours ago. All the serotonin that was in storage has been released, reabsorbed, and broken down. Your brain has run out of “happiness”. And the brain is slow when it comes to replenishing serotonin stocks. So even if you took more MDMA, you would not feel the same effects, simply because your brain has no more serotonin to release. This is why MDMA users often feel depressed after the effects of the drug go away and it takes them a little while to feel “normal” again. Those undergoing treatment for a mood disorder that involves anti-depressants are more likely to have a bad experience when using MDMA, especially if using MAOIs anti-depressants, as the combination may prove fatal.
As I said earlier, serotonin is mainly found in our gastrointestinal tracts. More and more research has found that, actually, our gut microbiota (those microorganisms that live inside our gastrointestinal system that we rely on to keep us alive) has some important effects on our brain health, also in issues related to serotonin levels. Gut microbiota is in charge of tryptophan metabolism, and therefore, serotonin production and regulation, and this can impact, not only locally at the gut, but brain neurotransmission. So, changes in our gut microbiota may reflect on our brain health and, of course, many factors can influence this, such as diet, culture, age and health issues, especially if taking antibiotics.
Blame serotonin for your poor decisions
Numerous studies link serotonin variation to disorders like schizophrenia, ADHD (attention deficit hyperactivity disorder), autism, bipolar disorder, compulsive behavior disorder, depression, and anxiety. Pretty much any disorder where social interactions are, somehow, different. Planning and decision-making have been also directly linked to levels of serotonin, meaning that depending on how much serotonin we have in our brains, we might be more prone to make poor decisions or might be more inclined to pursue short-term satisfaction to the detriment of a long-term solution.
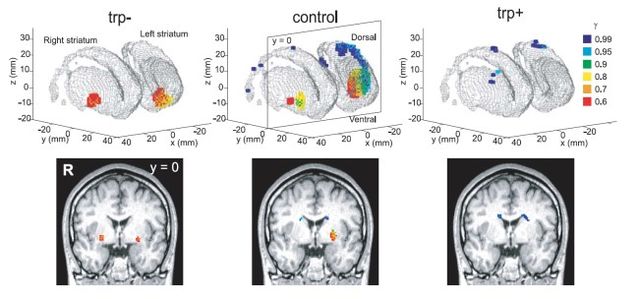
Brains were studied under different conditions (using trytophan, the serotonin precursor): reduction of tryptophan (trp-, meaning low serotonin), normal levels of tryptophan (control) and overload of tryptophan (trp+, meaning high serotonin). Cerebral blood flow was assessed by functional MRI. γ is the time scale for reward prediction, meaning that red, orange and yellow (smaller values) are related to short-term reward, whereas green, blue and purple (higher values) to long-term rewards. In this experiment, tryptophan depletion (i.e. low serotonin) is correlated to a more intense activation of short-term reward brain regions. On the contrary, tryptophan overload (i.e. high serotonin) seems to stimulate long-term reward brain areas.
Source: CC-BY, Tanaka SC et al., 2007
Apparently, serotonin is even responsible for our willingness to behave cooperatively or, otherwise, selfishly. Even a temporary reduction in serotonin may cause an inability to learn those altruistic behaviors that would (supposedly) make the world a nicer place for everyone. Serotonin also has the power of regulating our view of what is fair and how we react to subjectively unfair situations.
It is clear that serotonin is an important player in our mood and behavior. Nevertheless, it cannot be considered as the only answer to “regulate our happiness”. Environmental factors (the nature of our social interactions, learning, lifestyle, etc…) are essential pieces in the inner workings of our personality and our psychological wellness. So maybe, do not blame everything on your serotonin levels, but remember to be a little more empathic to those who struggle with heavy long-lasting serotonin reduction.
Comments