Disclosing About Health, Caring for One Another and Advocating = Gay Community
“The queer community is really good at this,” Snavely says, meaning regularly talking about health topics with friends and partners. He thinks there’s something special about the town’s legacy in gay culture, too. “Provincetown is a place where people came during the HIV and AIDS crisis to be sick, to die, to take care of each other — so that the lineage lives in this place.”
Dr. Daskalakis isn’t surprised at all this group of gay men stepped up. “Gay and other men who have sex with men’s relationship with public health has been tempered by fire into a new kind of trust,” he says. “People’s lives in that community have been saved by science and fueled by their own advocacy…. They were delivering this [information] to public health, and they had no problem doing it, because there was trust in that interaction.”
‘ENDING THE EPIDEMIC’
“The definition of ending HIV is a mathematical one,” Daskalakis explained. If New York City could get new infections down below 750 a year by 2020, he said new "transmission would no longer be fueling the epidemic."
When Daskalakis started work at the NYC Department of Health, he did so at a moment when it was suddenly possible, with proper inputs of political will and cold hard cash, to use antiretroviral drugs to engineer an end to HIV transmission in the city. The political will of Mayor Bill de Blasio and Governor Andrew Cuomo, he explained, helped secure the funding needed to scale up the distribution of expensive medications like Truvada.
Some of the language in this new HIV/AIDS prevention paradigm was coined by Daskalakis himself: “status-neutral care.” In an article in Open Forum Infectious Diseases, a medical publication, Daskalakis described status-neutral care as a “multidirectional continuum [that] begins with an HIV test and offers 2 divergent paths depending on the results; these paths end at a common final state,” which is the prevention of HIV transmission.
Daskalakis overhauled the city’s sexual health programs to make them status-neutral. STD clinics were renovated, streamlined and rebranded as “sexual health clinics.” “All the services had to look alike, whether you're HIV-positive or negative, and the idea was that if you come in and you are newly diagnosed with HIV you get started on meds on the same day of your diagnosis,” he explained. “If you are at risk for HIV, and you test HIV-negative, we don't dilly dally and wait. We start you PrEP that same day.”
Ad campaigns that had attempted to shame people out of contracting HIV instead distilled prevention down to a simple formula: “New boo? Get tested!” That’s because in the status-neutral-care continuum, getting tested is the first step to getting a patient enrolled in PrEP or TasP.
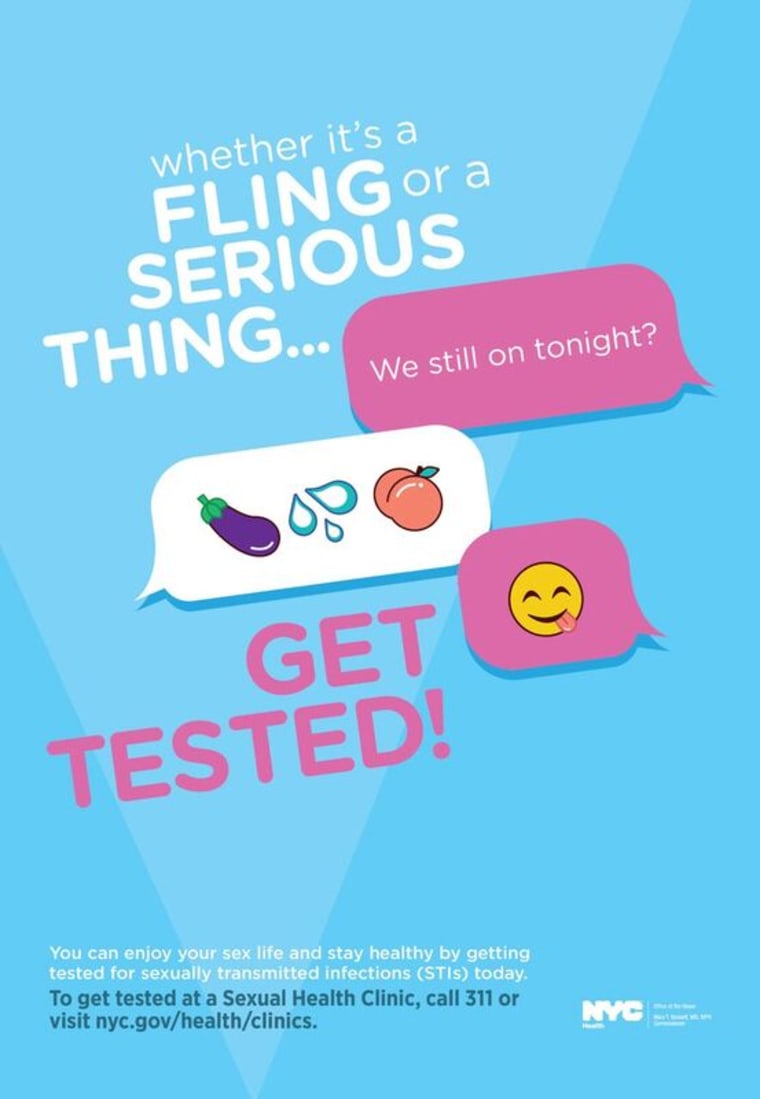 |
Gone were the scare-tactic campaigns of the Bloomberg administration (one infamous YouTube ad showed a close up view of anal cancer). They were replaced by joyful, brightly colored ads that encouraged people to come in for STD testing. Joining those ads were public awareness campaigns aimed at underserved communities with higher-than-average HIV incidence, like Spanish speakers, transgender women and heterosexual women of color. For the past several years, New York City subways and buses have been plastered with health department PrEP ads.
'REAPING THE BENEFITS'
The success of New York City’s revolutionary HIV prevention program is seen in the city’s declining rate of new HIV infections, but its success stark when compared to jurisdictions that haven’t implemented status-neutral care, or scaled up access to health care. The hotspots of HIV transmission today are in some of the poorest states that have refused to expand Medicaid, like Mississippi.
Daskalakis said his efforts prove the concept works, but he points to the challenges inherent in a model based on the distribution of expensive medications. “A lot of people doing this work are going from, ‘So now we can do it, we know we can,’ to 'How do you create sustainability?'”
Daskalakis describes the city’s new status-neutral-care regime as “the steam engine that's rolling through HIV in New York City and mowing it down in a pretty aggressive way.” “We're reaping the benefits by consistently seeing HIV incidence decrease,” he said. Last week, in an announcement of the record low HIV incidence, the City of New York said the new data shows it is on target to meet its Ending the Epidemic goals by 2020.

Comments